[et_pb_section][et_pb_row][et_pb_column type=”4_4″][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
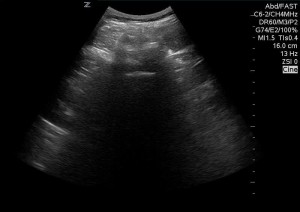
Lumbar punctures require properly identifying the L3/L4 or L4/L5 interspaces and placing a spinal needle between the spinous processes. In certain populations, including the obese, recognizing the anatomy may be difficult and ultrasound can be beneficial in reducing the number of failed procedures and repeated attempts. There are two general approaches for utilizing ultrasound when performing a lumbar puncture (LP). One can either use dynamic ultrasound guidance, visualizing the needle entering the dural space in real time. Alternatively, it can be used in advance to identify the proper landmarks and mark the position prior to the attempt, referred to static ultrasound guidance. Here is a step-by-step guide of the static ultrasound guided approach:
Please note that this is a demonstration on a volunteer. Proper sterile technique should be used at all times when performing this procedure.
Step-by- Step
- The patient may be placed in the sitting or lateral decubitus position, per the preference of the operator and the ability of the patient to sit still. The sitting position is preferred, if possible.

Patient in sitting position - Place a linear transducer (or curvilinear if patient is obese) in the transverse plane along Tuffier’s line (line connecting the superior iliac crests, corresponds to L4 vertebral body)

Probe on LP site - Center the probe over the spinous processes, the spinous process will appear as a crescent-shaped hyperechoic structure with posterior shadowing.
- Mark the midline directly above and below the probe.

Midline on the probe is marked with a marking pen 
A mark above and below the probe, shown after probe removal - Rotate the probe 90° into the sagittal plane (probe marker towards patient’s head)
- Center the probe over the interspinous space with two spinous processes visible on either side.


- Mark the midline directly to the right and left of the probe

After marking the midline of the probe in the sagittal plane. 4 markings are now seen. - Extend the transverse and sagittal markings until they connect; the point of intersection represents the middle of the interspace and the location to insert the spinal needle.

Connection between the markings. The needle is inserted on the X - Ensure that the patient does not move after marking the skin and perform the LP as soon as possible.
Discussion:
Nomura, et al.[i], studied the utility of ultrasound-assisted lumbar punctures in the adult population. They conducted a randomized, prospective, double-blind study in the emergency department of a teaching institution, assessing whether ultrasound landmark identification would increase the success of attempted LPs and ease their performance. 46 patients were included in the study, 12 were obese with BMI >30. Ultrasound landmarks were identified by a study investigator and marked with UV ink by a study investigator. The LP operator then identified the landmarks using the traditional blind technique and marked it with different UV ink. The patient was then randomized to landmark versus ultrasound guided LP and the study investigator marked the appropriate previously identified location using visible ink and the operator performed the LP. 1/24 ultrasound assisted LPs failed, as opposed to 6/22 in the traditional landmark group, RR 1.32; 95% CO 1.01-1.72. All five of the obese patients in the ultrasound group had successful LPs, while 4/7 failed in the palpation group. The study is limited due to its’ small sample size, resulting in only 12 obese patients and a significantly older obese cohort in the palpation group (41.9 years vs. 30.6 years). It is interesting that there was such a high success rate even though significant time had passed since the original US landmark had been marked.
Conclusion:
Ultrasound seems like it would be a promising tool to assist in the difficult LP. Indeed, the study results show favorable evidence that ultrasound can help improve success rates in patients whose anatomy is difficult to identify. However, given the small study size it is difficult to tell how generalizable the study results really are. Ultrasound is a great tool to have in our arsenal when faced with a challenging LP, but more studies are necessary before it can be introduced as a first-line everyday evidence-based practice tool.
[i] Jason T. Nomura et al., “A Randomized Controlled Trial of Ultrasound-Assisted Lumbar Puncture,” Journal of Ultrasound in Medicine 26, no. 10 (2007).
This post reviewed and edited by Dr. Josh Guttman
[/et_pb_text][/et_pb_column][/et_pb_row][et_pb_row][et_pb_column type=”1_2″][et_pb_team_member admin_label=”Person” name=”Raphi Bollag, MD” position=”Author” image_url=”http://theempulse.org/wp-content/uploads/2015/11/Raphael-Bollag.png” animation=”off” background_layout=”light” twitter_url=”https://twitter.com/RaphiBollag” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Dr. Bollag is a categorical Emergency Medicine resident at the LIJ Medical Center.
[/et_pb_team_member][/et_pb_column][et_pb_column type=”1_2″][et_pb_team_member admin_label=”Person” name=”Dr. Josh Guttman, MD, FRCPC” position=”Reviewer and Ultrasound Editor – theEMPulse.org ” image_url=”http://theempulse.org/wp-content/uploads/2015/10/Guttman-e1453253661766.jpg” animation=”off” background_layout=”light” twitter_url=”https://twitter.com/josh_guttman” use_border_color=”off” border_color=”#ffffff” border_style=”solid” saved_tabs=”all”]
Dr. Guttman graduated from the at Mt. Sinai Medical Center Emergency Ultrasound Fellowship and is now an Attending Physician at the LIJ Division of Emergency Ultrasound.
[/et_pb_team_member][/et_pb_column][/et_pb_row][/et_pb_section]