[et_pb_section admin_label=”section”][et_pb_row admin_label=”row”][et_pb_column type=”4_4″][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
The Case:
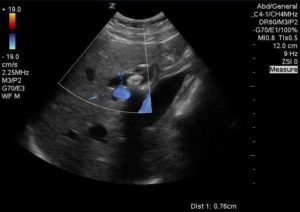
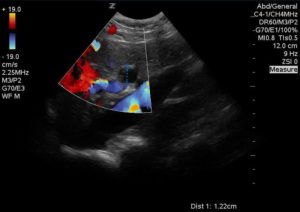
A 41-year-old female with no prior medical history presents to the ED with one day of severe right upper quadrant pain that began after eating. She had nausea, but no vomiting and endorsed chills. Vital signs were within normal limits. On exam her abdomen was soft with right upper quadrant tenderness, but no rebound, guarding, or Murphy’s sign The ED ultrasound team was called to complete an ultrasound examination of the right upper quadrant to evaluate for cholecystitis.
The following images were obtained:
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
DILATED COMMON BILE DUCT
[/et_pb_text][/et_pb_column][/et_pb_row][et_pb_row admin_label=”Row”][et_pb_column type=”4_4″][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Case Outcome
Blood testing revealed a WBC count of 7.1, Alkaline Phosphatase level of 202u/L, AST (SGOT) of 363u/L, ALT (SGPT) of 289u/L and total bilirubin 1.5mg/dL. The patient was admitted to the surgery service. Repeat abdominal ultrasound revealed cholelithiasis and choledocholithasis without signs of cholecystitis. The patient underwent ERCP that revealed numerous CBD stones.
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Discussion:
It has been established that emergency physicians are proficient at identifying cholelithiasis and cholecystitis in patients with a high pre-test probability. A systematic review published in 2011 demonstrated a sensitivity of 89.8% and a specificity 88.0% for the diagnosis of cholelithiasis by emergency bedside ultrasound. An additional study published in the Annals of Emergency Medicine found that trained Emergency Physicians had a sensitivity of 87% and specificity of 82% for diagnosing cholecystitis with POCUS, which was comparable to radiology ultrasound (83% and 86%, respectively.)
Choledocholithiasis is a more challenging diagnosis. Direct visualization of stones and CBD enlargement > 6mm are the songraphic findings of choledocholithiasis. However it can be difficult for the novice sonographer to identify and measure the CBD. More importantly, these findings are not universal. A single center retrospective chart review published in 2014 found that among 111 cases of choledocholithiasis, only one case had a dilated CBD without additional sonographic or laboratory abnormalities. All of the patients with common bile duct stones without CBD dilatation on ultrasound had abnormal lab values. The authors of that study suggest that omission of the CBD measurement is unlikely to result in a missed case of choledocholithasis, as long as the rest of the exam is normal.3
At this time no high quality data exists to support the use of LFTs and ultrasound for the diagnosis of choledocholithiasis. A Cochrane Database Systematic Review from 2015 comparing ultrasound and LFTs for the diagnosis of choledocholithiasis found only poor quality studies that evaluated the accuracy of these modalities for the diagnosis of choledocholithiasis.4 The systematic review included five studies that compared the accuracy of ultrasound with surgical findings and one study that compared abnormal LFTs with surgical findings. Sensitivities for ultrasound diagnosis of choledocholithiasis ranged from 32-100% with specificities ranging from 77-97%. The one study that evaluated the accuracy of abnormal LFTs in diagnosing choledocholithiasis also evaluated the accuracy of ultrasound findings. The sensitivity for ultrasound in that study was 32% when compared to 84% and 92% for elevated bilirubin and alkaline phosphatase, respectively.
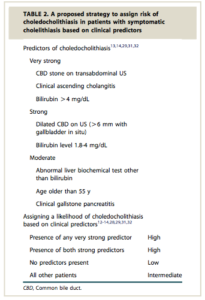
Given these results further testing should be pursued in patients with a high clinical suspicion for choledocholithiasis and otherwise negative work-up. The American Society For Gastrointestinal Endoscopy practice guidelines for evaluating suspected choledocholithiasis recommend risk-stratifying patients based off criteria in the table to the right.
Patients at high risk for choledocholithiasis should be admitted for further evaluation with gastroenterology. Both endoscopic ultrasound and magnetic resonance cholangiopancreatography (MRCP) are appropriate follow-up tests for those with intermediate risk, with numerous systematic reviews showing no statistical difference between the diagnostic utility of the two.5,6,7 Ultimately, confirmed bile duct stones are removed with sphincterotomy during Endoscopic Retrograde Cholangio Pancreatography (ERCP).
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Conclusion:
Point of care ultrasound has a reasonably good diagnostic accuracy for Choledocholithiasis. A positive finding (dilated CBD or stone in the CBD) in the right clinical context should lead the physician to further purse the diagnosis with more advanced modalities such as MRCP. However, Ultrasound alone cannot exclude choledocholithiasis and further research needs to be conducted in regards to its utility in the ED. All patients with a suspected CBD stone should undergo laboratory testing and RUQ ultrasound. More advanced imaging should be pursued if clinical suspicion persists even in the setting of negative imaging. If the patient’s labs are within normal limits and a RUQ ultrasound is otherwise normal it is unlikely that the patient has a CBD stone, even if the CBD measurement cannot be obtained. Patients with stones in the CBD should be admitted for further management. ERCP remains the definitive treatment of choledocholithiasis.
[/et_pb_text][et_pb_text admin_label=”Text” saved_tabs=”all” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid” global_module=”3014″]
Disclaimer: All cases discussed on this site are composites, representative of specific clinical situations, and not based off of any individual patient. Any similarities to actual persons are coincidental.
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
References:
- Ross M, Brown M, Mclaughlin K, et al. Emergency physician-performed ultrasound to diagnose cholelithiasis: a systematic review. Acad Emerg Med. 2011;18(3):227-35.
- Summers SM, Scruggs W, Menchine MD, et al. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med. 2010;56(2):114-22.
- Becker BA, Chin E, Mervis E, Anderson CL, Oshita MH, Fox JC. Emergency biliary sonography: utility of common bile duct measurement in the diagnosis of cholecystitis and choledocholithiasis. J Emerg Med. 2014;46(1):54-60.
- Gurusamy KS, Giljaca V, Takwoingi Y, et al. Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev. 2015;(2):CD011548.
- Verma D, Kapadia A, Eisen GM, Adler DG. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64(2):248-54.
- Giljaca V, Gurusamy KS, Takwoingi Y, et al. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. Cochrane Database Syst Rev. 2015;(2):CD011549.
- Ledro-cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangio-pancreatography? A systematic review. Eur J Gastroenterol Hepatol. 2007;19(11):1007-11.
- Maple JT, Ben-menachem T, Anderson MA, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9.
[/et_pb_text][/et_pb_column][/et_pb_row][et_pb_row admin_label=”row”][et_pb_column type=”1_2″][et_pb_team_member admin_label=”Person” name=”Jennifer Larson, MD” position=”Author” animation=”off” background_layout=”light” use_border_color=”off” border_color=”#ffffff” border_style=”solid” image_url=”http://theempulse.org/wp-content/uploads/2016/04/larson.jpg”]
Dr. Larson is a resident in the Combined Emergency Medicine/Internal Medicine/Critical Care program at the LIJ Medical Center.
[/et_pb_team_member][/et_pb_column][et_pb_column type=”1_2″][et_pb_team_member admin_label=”Person” name=”Dr. Josh Guttman, MD, FRCPC” position=”Reviewer and Ultrasound Editor – theEMPulse.org ” image_url=”http://theempulse.org/wp-content/uploads/2015/10/Guttman-e1453253661766.jpg” animation=”off” background_layout=”light” twitter_url=”https://twitter.com/josh_guttman” use_border_color=”off” border_color=”#ffffff” border_style=”solid” saved_tabs=”all”]
Dr. Guttman graduated from the at Mt. Sinai Medical Center Emergency Ultrasound Fellowship and is now an Attending Physician at the LIJ Division of Emergency Ultrasound.
[/et_pb_team_member][/et_pb_column][/et_pb_row][/et_pb_section]