This guide was created to help assist ED providers being pulled to help in ICUs during the COVID pandemic. The majority of the information here is applicable to general ICU care however some is specific to COVID. The last section in the document serves as a summary and daily checklist. A PDF daily rounding checklist is attached as well.
COVID Labs and Imaging
| Labs on Admission to ICU -CBC with differential -Comprehensive metabolic panel -Magnesium -Phosphate -Coagulation panel (PT/ aPTT/ INR) -D-Dimer -Procalcitonin -C-reactive protein (CRP) -Lactate dehydrogenase (LDH) -Ferritin -Creatine kinase (CK/ CPK) -Arterial blood gas with lactate |
Daily Labs AM: CBC with differential – CMP, Mg, Phos – ABG with lactate – Procalcitonin PM: ABG IF ON CVVHD add to the above: -BMP, Mg, Phos every six hour |
| Labs every Mon, Wed, Fri – D-Dimer -LDH -Ferritin -CK -Coagulation Panel -Troponin -CRP -Triglycerides and lipase if on propofol |
Imaging Chest X-Ray -On admission to ICU. After central line placement. Acute change in oxygenation while intubated. At the discretion of ICU Team. All other imaging at the discretion of ICU Team |
Ventilation Management and Troubleshooting
Initial vent management
Mode: Assist Control
Tidal volume (TV): 6mL/kg ideal body weight
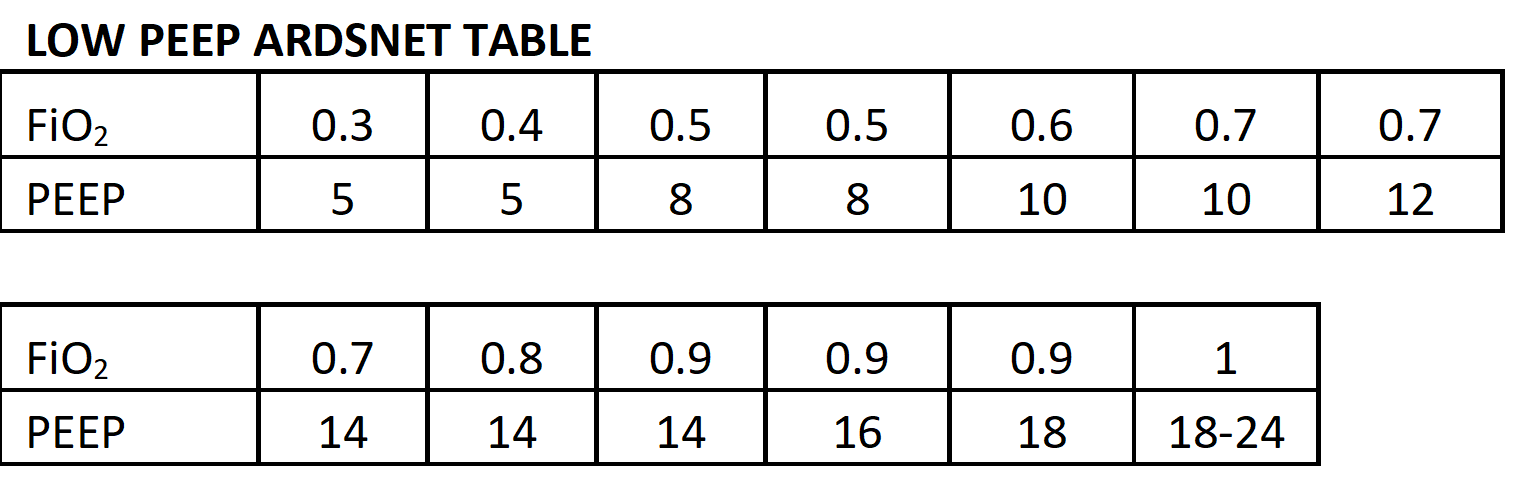
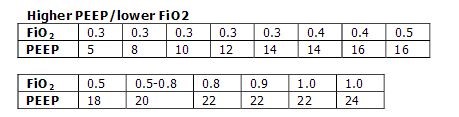
Rate: 26 bpm (consider 28-30 if known pH<7.20) FiO2: 100% PEEP: start at 5 (10 if BMI >35), titrate PEEP and FiO2 using ARDS low PEEP if BMI <35 and high PEEP table if BMI >35 to O2 saturations 88%-96%, PaO2 >55
Plateau Pressure: After patient oxygenating well check plateau pressure if <30 no further adjustments needed. If >30 see plateau trouble shooting below.
ABG: Send ABG 30-45 min after adjusting settings
PIP: Peak Inspiratory Pressure, is an indicator of large airway pressures. Ideally should be less than 40. An acute increase may indicate ETT kinking or dislodgement (Rt mainstem), pt biting, mucous plugs, severe dyssynchroncy.
pH Management
- If pH <7.15 increase RR until >7.15 or PaCO2 <25 (max RR 35)
- Recheck ABG in 45 min
- If ABG now with pH ≥ 7.15 can titrate RR to keep pH < 7.2 no additional changes need to be made to the Vt
- If ABG with pH < 7.15 increase tidal volume by 1cc/kg to ≤ 8cc/kg ideal body weight
- Recheck plateau pressure after adjusting Vt, needs to be ≤ 30, if >30 decrease Vt until ≤ 30
- If unable to keep plateau pressure ≤ 30 and pH ≥ 7.2 follow steps in hypoxia management for desynchrony and proning
- If unable to keep pH ≥ 7.2 escalate to critical care attending, may consider ECMO consult
- On occasion, a bicarb bolus or infusion maybe considered if renal function is relatively preserved to counteract pH<7.0
Hypoxia Management – Initial after intubation
- Titrate PEEP and FiO2 using ARDS net tables as above goal SpO2 88%-96%, PaO2 >55
- Check plateau pressure with each change in PEEP and see plateau pressure troubleshooting below if > 30
- Consider changing to high PEEP table in patients with BMI <35 since some COVID patients seen to be highly PEEP responsive.
- If patient dyssynchronous with vent increase level of sedation to achieve RASS -4 to -5 (see sedation below)
- If continued dyssynchrony despite RASS -4 to -5 procced to paralysis (see below)
- If P/F ratio <150 on FiO2 > 60 with optimal settings and vent synchrony patient should be proned
- Ensure adequate resources (staff, RT, proning lead, proning pillow, proper draping, etc.) prior to proning, protect ET tube and central lines
- Prone patient for 16 hours on 8 hours off (ideally, timed for prone from PM to AM)
- Continue as long as P/F ratio <150 while supine
- If still hypoxic consider critical care attending input for further interventions such as recruitment maneuver, APRV, ECMO consult
Hypoxia Management – Acute in a previously stable intubated patient
- Troubleshoot using DOPE mnemonic
- Dislodged – Check EtCo2 for good waveform, check for BL “symmetric” breath sounds, pleural sliding on lung US, if necessary may visualize ET tube placement with laryngoscopy
- Obstruction – Attempt to pass suction catheter through entire length of ET tube, if unable may need tube exchange or emergent fiberoptic bronchoscopy
- Pneumothorax – Listen for BL “symmetric” breath sounds, ultrasound, STAT chest xray, if high suspicion and patient decompensating perform finger thoracostomy
- Equipment– Ensure O2 wall connection to vent, check vent tubing to ETT. Listen for leaks, fasten connections, ask RT for help (don’t disconnect from vent)
- Optimize volume status with diuresis or RRT if patient not making urine
- If patient remains hypoxic without acute cause identified then consider bedside echo to rule out massive PE. If not consistent, then follow steps above for initial hypoxia management.
Plateau pressure troubleshooting
- Plateau pressure should be checked with every change in Vt, PEEP, or if patient has worsening oxygenation
- If having issues with plateau pressures > 30, first confirm: adequate sedation, no dyssynchrony, net negative/even fluid balance
- If confirmed above and plateau pressure > 30 decrease Vt by 1 cc/kg ideal body weight until plateau pressure <30 (minimum 4cc/kg) resend ABG in 45 minutes to evaluate effect on pH
- If p-plat still >30, decrease inspiratory time (i-time) to 0.4-0.5 sec
- Recheck p-plat 1-2 mins after change to ensure <30, if not consider paralytics if dyssynchrony exists (over breathing the set RR, breath stacking, larger Vt than vent setting)
- If despite perfect synchrony with ventilator, p-plat>30, decrease PEEP by 2, recheck p-plat until p-plat <30, or pt derecruits (acute desaturation <88% or significant hemodynamic changes)
- Consider intraabdominal hypertension as uncommon cause, check bladder pressures (less than 14 normal).
- Use pH management section above once plateau pressure < 30
- If plateau pressure < 25 and having trouble with vent synchrony, may increase TV by 1cc/kg until patient at 6cc/kg ideal body weight or plateau pressure >25
- If plateau pressure < 30 and patient is breath stacking or dyssynchronous, then increase Vt by 1cc/kg until: patient no longer breath stacking/dyssynchronous, or you reach 8cc/kg, or plateau pressure equals 30
Additional Consideration
- Monitor vent tracings for signs of air trapping and consider checking for significant Auto-Peep when RR >30.
- Unless absolutely necessary, disconnecting patients from ventilator should be avoided, due to aerosolization risk and significant derecruitment. Even in cardiac arrest, pt may still be mechanically ventilated, but RR should be reduced to less than 18.
Ventilator Weaning and Extubating
Vent Weaning
- All patients who are able should be considered for daily spontaneous awakening trial, which consists of turning off sedation to achieve RAS 0. This should be done if the patient meets the following criteria:
- Not proned for over 48 hours
- Off of any paralytics for minimum of 24 hours
- Hemodynamically stable requiring minimal pressors
- SpO2 >92% or PaO2 > 75 with FiO2 ≤ 50% and PEEP ≤ 10
- If meets criteria for SAT once RAS ≥ -2, all patients should also be considered for daily spontaneous breathing trial if they meet the following additional criteria:
- Not requiring RASS < -2 to achieve vent synchrony
- Ventilator rate set ≤ 30 and patient’s spontaneous respirations ≤ 35
- Discuss appropriateness of SBT if patient meets criteria to assess readiness for extubation.
- Change ventilator mode to CPAP with pressure support of 10 and peep of 5-8, can base these initial settings off patient’s current AC settings. Ideally should be on CPAP 5/5 prior to extubation.
- SBT should be continued for 120 minutes unless patient fails prior to this time. Patient has failed the SBT and it should be stopped if any of the following criteria are met:
- Increased WOB or RR > 5+pt’s RR on vent sustained for 5 minutes
- SpO2 <92%
- Vts persistently lower than expected (< 5 cc/kg ideal body weight)
- Heart rate >140 or 25% above baseline HR
- Worsening agitation, anxiety, or discomfort
- Rapid shallow breathing index > 105 (use vent parameters, calculate on MDCalc.com)
- If patient fails place back on full support and re-sedate as necessary for comfort and vent synchrony
- If patient has successful SBT for 120 minutes then send ABG to evaluate for pH, PCO2.
- If ABG not significantly worsened during SBT, extubation readiness should be discussed during rounds. Decision to extubate is the purview of the critical care attending.
- Calculate rapid shallow breathing index before moving on. RSBI = breaths/min/L or f/Vt, can use MdCalc of vent to do this for you.
- <105 likely successful wean to extubation (97% sensitive)
- >105 likely to fail extubation
Extubation Readiness and Process
- Confirm completion of the Vent Weaning section above and confirm that patient is breathing spontaneously
- Extubation should be performed if the following additional criteria are met:
- RASS 0 to -1
- Able to follow commands
- Intact cough reflex (pass suction catheter to distal ET tube and confirm induces coughing)
- Minimal airway and oral secretions (suctioning less than Q2)
- FiO2 ideally <40%
- Optimized volume status
- If CPAP settings >5/5 but consistently passing SBTs consider extubation to BiPap
- Evaluate for cuff leak especially if patient intubated >6 days
- Suction all oral secretions. Set vent back to full support and record Vt delivered. Deflate ET tube cuff and monitor volume delivered for 6 breaths. A decrease of at least 10% in delivered Vt suggests minimal supraglottic swelling.
- If there is less than a 10% decrease then there is no cuff leak. This means there is likely supraglottic swelling that will result in stridor after extubation. In this case pretreat with dexamethasone 0.15 mg/kg or methylprednisolone 20 mg 4 hours prior to extubation. No need to repeat cuff leak test prior to extubation.
- If patient meets all of above criteria they should be extubated.
- Remove OG tube and replace with NG/feeding tube prior to extubation. Place speech and swallow consult in sunrise and remove NG when able.
- Place extubation order in sunrise and speak with RT who will come to extubate the patient, but the following is the basic procedure:
- Set up suction, intubation equipment if high risk extubation,
- Place patient on NC O2 or have NIV ready if extubating to BiPap/HFO2
- Remove ET tube securing devices
- Suction mouth
- Deflate ET tube cuff and remove tube
Sedation and Paralysis
- Intubated patients should be placed on both an analgesic and a sedative agent. When increasing doses or starting a new agent you should include an appropriate weight-based bolus prior to initiating the drip (with the exception of Precedex).
- Target RASS should be -4 to -5 in acute ARDS phase and 0 to -1 when P/F ratio above 300
- Always consider the indication for sedation when choosing a sedation package
- If attempting to achieve vent synchrony use agents that suppress respirations (Fent, Prop)
- If you need analgesia and are tying to wake the pt up for SBT use agents that do not suppress respirations (Precedex, low dose ketamine > 0.5mg/kg/min)
- Our recommended starting sedation package post intubation for adequate sedation, amnesia and analgesia is the following: Fentanyl 1 mcg/kg/min, Ketamine 0.5 mg/kg/hr, Propofol 30 mcg/kg/hr. Ketamine should be titrated off first, then propofol exchanged for precedex and then fentanyl titrated off when attempting SAT.
Analgesic Agents
- First line should generally be Fentanyl 0.5 – 3 mcg/kg/hour IV infusion
- Fentanyl preferred in renal dysfunction.
- Caution in liver dysfunction, concern for serotonin syndrome, or in obesity due to lipophilicity.
- Morphine 0.1 – 0.5 mg/kg/hour IV infusion
- Should not be used in patients with severe renal dysfunction.
- Dilaudid 0.5 – 2 mg/hour IV infusion
- Should not be used in patients with severe renal dysfunction
- Consider changing patients on longer term fentanyl (2-3 days )or those receiving high (>250 mcg/hr) fentanyl doses to dilaudid.
- If titrating up on analgesic medications, consider PRN order of 50 mcg fentanyl IV or 4 mg morphine IV instead of increasing infusion
- Utilize adjunctive therapies early (standing acetaminophen or gabapentin)
Sedation Agents
- First line should be Propofol 10-50 mcg/kg/min IV infusion or Precedex 0.2-1.5 mcg/kg/hr IV infusion.
- If using propofol monitor Triglycerides and lipase every 48 hrs, if Triglycerides >500 consider dose reduction. If Triglycerides >1000 or developing pancreatitis discontinue. Aim Propofol dose <20mcg/kg/min by day 3, and transition to other meds by day 6 of ICU.
- Precedex preferred if only light sedation required or nearing extubation. Lack of respiratory suppression makes this less optimal if having issues with vent synchrony.
- Precedex can induce bradycardia and cause liver dysfunction. Higher doses cause more bradycardia so if struggling with bradycardia consider reducing infusion rate or changing agents.
- Second line should be Midazolam 0.25 to 1 mcg/kg/min IV infusion.
- Should be utilized if unable to achieve deep sedation with RAS -5 and vent desynchrony prior to initiating paralysis.
- Caution with long term infusion at high dose rates especially in obesity, will accumulate in the tissue resulting in prolonged sedation and difficulty weaning.
- Do not abruptly discontinue if prolonged infusion, may initiate withdrawal. Consider long acting oral benzodiazepines as bridging/weaning.
- Ketamine 0.1 – 2 mg/kg/hr IV infusion
- Keep in mind that Ketamine has different effects at different doses. On the lower end <0.5 ketamine infusion likely effective analgesia, 0.5-1.25 ketamine likely leads to hallucinations and agitation, >1.25 ketamine will cause full dissociation. Keep this in mind when trying to wean ketamine, patients will metabolize back through the hallucinogen dose and become agitated, this can be fixed by increasing the ketamine if you want the patient unconscious or by using a one time benzo push if you are trying to turn it off.
- Give adequate 1.5-2 mg/kg bolus prior to initiating infusion to ensure non-sub dissociative dose.
- Can cause reflex hypertension and tachycardia.
- Multimodal Analgesia:
- Consider acetaminophen IV/PO standing doses if not tracking fevers
- Consider quetiapine if QTc <500. Higher nighttime doses avoid over sedation at night with Propofol/opioids. Start 25 mg bid, increase night dose first.
- Consider long acting benzodiazepines if midazolam infusion present. Clonazepam 1-2 mg daily, titrate to be able to wean off infusion.
- Consider neuroleptics if Qtc <500. Haloperidol 2-5mg IV, Olanzapine 5mg IV
- Consider instituting oxycodone or methadone in patients on opioid infusions for over 3 days for successful weaning off infusion. Methadone (QT prolonging) 5mg q8hrs, Oxy 5 q4hrs standing.
- In refractory cases, consider Phenobarbital loading IV/PO with rapid taper similar to ETOH withdrawal regimen
Paralytics
- If requiring paralysis dose of paralytic infusion should be titrated to lowest possible dose using Train of Four and vent synchrony. Patient should have minimum 2/4 train of four while on drip, if able to achieve higher train of four and maintain vent synchrony this is ideal, paralytic should be discontinued as soon as possible. If TOF not available, vent synchrony should be the target.
- Daily trial off paralytics to determine if RASS -5 alone enough to keep patient synchronous with vent.
- Ensure RAS -4 to -5 prior to initiation of paralytic as these agents do not provide any sedation or analgesia
- Caution in using steroids in paralyzed patients as this increases risk of severe myopathy
- First line should be Cisatracurium (Currently on shortage)
- Bolus Cisastracurium 0.2mg/kg IV x 1. Continuous infusion: 1-3 mcg/kg/min IV infusion.
- Hoffman Elimination and therefore preferred agent in renal and liver failure
- Second line should be Rocuronium if Cisatracurium unavailable
- Bolus Rocuronium 1mg/kg. Continuous infusion 8-12 mcg/kg/min.
- Alternatively, may consider intermittent bolus dosing of 1mg/kg every 2-3 hours, especially if not expected to need prolonged paralysis.
- Excretion somewhat impaired by renal and liver failure
Hemodynamics and Fluid Management
Fluid Balance
- Conservative fluid strategy, attempt to keep patient even to slightly net negative. Review I&Os daily to achieve this goal. Pay attention to past several days, as diuresis is frequently initiated early in these patients.
- Avoid maintenance fluids, unless for an explicit reason (e.g. hypernatremia)
- Preform daily bedside POCUS to assess LV function and RV size. Consider LVOT VTI measurement and IJ variation at 90 degrees to further evaluate volume status.
- LVOT VTI >22 cm/s suggests non-volume responder. <18 suggests volume responsive
- R internal jugular respiratory variation with the patient at 90 degrees <12% suggests non-volume responder. >25% suggests volume responsive.
- Attention: fluid responsiveness is not equal to hypovolemia. If stable hemodynamics and physical exam euvolemic, do not administer IV fluids.
- If clinical assessment suggests hypovolemia and fluid responsive US then should give fluid bolus.
- Lactated ringers should be the first line resuscitation fluid.
- Normal saline is 2nd choice
- Colloids such as albumin are rarely helpful unless there is a specific indication
- Discuss during rounds plan for diuresis along with net balance goals daily. Check I/O balance regularly to ensure reaching the goal.
- If patient not requiring pressors should order standing Q12H lasix dose based of off creatine x 40
- If minimal pressor requirements (likely sedation related) order standing Q24H lasix dose creatinine x 40
- If significant pressor requirements do not place on standing Lasix
- If patient not making adequate urine despite standing diuretics or unable to tolerate Lasix due to hypotension or worsening AKI and becoming more net positive consult nephrology for initiation of HD or CRRT.
- Persistent metabolic acidosis, uremic encephalopathy, refractory hyperkalemia, hypervolemia interfering with oxygenation are other indications for CRRT/HD.
Shock Management
- If MAP < 65 attempt to identify cause of shock (hypovolemic vs septic vs cardiogenic)
- Bedside US (effusion, tamponade, volume status, EF, SV) immensely helpful
- First line pressor should be Levophed 0.05 – 1.0 mcg/kg/min IV infusion
- Add Vasopressin 0.03 units/hr IV infusion if levophed >0.15mcg/kg/min for >1hr
- If persistent hypotension consider fluid status as above with POCUS assessment
- If significant RV dilation consider PE as cause of hypotension
- Consider tPA in refractory shock, 50mg with 10mg bolus and 40mg 1hr infusion.
- If significant LV dysfunction consider cardiogenic shock
- Ensure any negative inotropes are discontinued such as beta-blockers, CCBs, or any antihypertensive medications
- Initiate inotropic support with dobutamine infusion 2 mcg/kg/min and titrate up by 1-2 mcg/kg/min.
- Dobutamine may induce tachydysrhythmias so use with caution in the already significantly tachycardic patient or consider another agent such as Milrinone.
- Dobutamine reduces systemic vascular resistance so if shock not due to reduced LV function will result in worsening hypotension.
- Epinephrine is an excellent inotropic agent at lower doses (0.05-0.2 mcg/kg/min) for cardiogenic shock
- Check SVO2, lactate Q1-2 hrs to gauge response to therapy
- If worsening despite inotropic support, consider consulting ECMO team.
- If significant RV dilation consider PE as cause of hypotension
Prophylaxis and Tube Feeds
VTE Prophylaxis
- If creatinine clearance greater than 30: Lovenox 40 mg q24 or Lovenox 40 Q12H if BMI >30
- If creatinine clearance less than 30: Heparin 5000 units q8
- Mechanical prophylaxis with venodynes on all patients unless contraindicated, as available
- If patient unable to receive chemoprophylaxis, intermittent compressive device should be maintained.
- Consider full dose AC if D-dimer >5x upper limit of normal and signs of PE.
GI Prophylaxis
- Stress ulcer prophylaxis should be used in all patients who are intubated
- If creatinine clearance greater than 30: Famotidine 20 mg q12
- If creatinine clearance less than 30: Famotidine 20 mg q24
- Avoid constipation especially in setting of prolonged narcotic use, goal BM every 48-72 hours.
- If no bowel movement for >24 hours after initiation of enteral feeding place patient on standing medications
- Give senokot 2 tabs by OG BID, Miralax BID
- If no bowel movements, may add suppository (Bisacodyl)
- If still no bowel movement in 24 hours add lactulose 30 mL once daily
- If still no bowel movement in 24 hours check for rectal impaction, give mineral oil enema PR and repeat x 1 in 4-6 hours
- If still no bowel movement in 24 hours consider obstruction, reduce narcotics, methylnaltrexone trial, consider GI consult.
Tube Feeds
- Evidence suggests that enteral feeds should be started within 24-48 hours of intubation.
- The only real contraindications to tube feeds are bowel obstruction, perforation, major GI bleeding.
- Relative contraindications are peri-extubation or procedure, minor GI bleed, profuse diarrhea, very high dose vasopressors.
- The registered dietitian on the unit will help with the majority of tube feeding issues but here are some of the basics.
- Calorie goal is generally 25 kCal/kg/day and 1.5 grams/kg/day protein. Feeds should be started at 25-50% caloric goal and increased over 3 days.
- Always initiate enteral feeding at trophic dose (10cc/hr continuous or 50cc q6hrs intermittent)
- Feed type selection is based off of patient caloric needs and medical comorbidities, Vital-AF generally fine but dietary can provide guidance here
- Major categories of enteral feeds are for renal impairment, diabetes, cardiac, elemental (poor enteral absorption)
- Don’t forget to include water flushes with tube feeds to prevent hypernatremia and other electrolyte abnormalities. Online calculators can be used to give you the amount of daily free water flushes needed. If patient is developing hypernatremia the first thought should be inadequate free water so additional flushes can be given via OG.
- If patient on high dose propofol don’t forget that this can lead to significant overfeeding and tube feeds should be adjusted accordingly.
COVID ICU Daily Rounding Checklist
Neuro
- Can patient undergo daily SAT?
- No – Because one of the following [ ] proned [ ] on paralytics within last 6 hours or train of four not 4/4 [ ] Hemodynamically unstable more than minimal pressors [ ] SpO2 <92% [ ] PaO2 < 75 [ ] FiO2 > 50% [ ] PEEP > 10
- Yes – perform SAT by pausing sedation
- If paralyzed daily trial off of paralysis
- Mental Status: assess RASS, if RASS >-3 assess for CAM-ICU: managing delirium (non pharmacologic + pharma) (Hint: MDCalc.com has both RASS, CAM-ICU)
- Review current doses of sedation medications and de-escalate as tolerated for vent synchrony (infusions -> intermittent -> enterals -> wean off)
- Acute change in mental status: consider head CT, EEG
CV
- Observe Current MAP
- Attempt to reduce current dose of vasopressors if MAP >65, compare to prior dose and re-evaluate causes of shock if dose increasing
- Daily POCUS assessment of volume status (see fluids section for further details)
Resp
- If able to perform SAT, can patient undergo daily SBT?
- No – Because one of the following [ ] Requiring RASS < -2 to achieve vent synchrony [ ] vent rate set > 30 [ ] patients spontaneous respirations > 35
- Yes – Perform SBT as described above
- Review Vent settings (mode / rate / Vt / FiO2 / PEEP), p-plat, P/F ratio
- Confirm safe ventilator settings, 6cc/kg ideal body weight, plateau pressure <30 (see vent section for further details)
- Review last ABG
- Order CXR (only if there’s a clinical change OR actively managed chest tubes)
- Palpate chest wall and neck to rule out subcut emphysema as early sign of pneumothorax in high airway pressure patients
GI
- Confirm with RN that patient is tolerating Tube feeds (residuals?)
- Examine the patient’s abdomen, tender? Overdistended?
- Make sure patient has stress ulcer prophylaxis as above
- Check with RN for last bowel movement and if not achieving goal of 1 BM ever 24-72 hours follow prophylaxis section above
GU
- Review I/O’s for the last 24 hours, goal even or net negative as described above
- Confirm that patient is on appropriate diuretics dosing based on fluids section above
- Review BUN / Creatinine, electrolytes, and last creatine kinase
Heme
- Confirm that patient is on appropriate VTE prophylaxis as listed above
- Review hematocrit, platelets count (and trends, HIT?), and abnormal coags
- Review last D-dimer, LDH, and ferritin
- Consider therapeutic AC in patients with increasing inflammatory markers and stable Hg or those on dialysis
- Consider screening LE dopplers for increasing LE edema
ID
- Review antibiotics (antibiotic/ indication / dose / day #), have plan to de-escalate or discontinue antibiotics based on empiric duration, cultures, or change in clinical status
- Review daily procalcitonin and consider adding additional coverage if increasing rapidly
- Review culture results and re-culture if change in clinical status or not responding to treatment
- Monitor fever trends. Pay particular attention to fevers after 1st week, in setting of hemodynamic instability, or progressive vent support need.
- Patients frequently followed by ID service, review their daily notes.
Endo
- Review glucose and insulin dose (inf + intermittent sliding scale + long acting)
- Adjust sliding scale for patients with poorly controlled blood sugars (should be 140-200)
- If blood sugar >200 x2 and clinically worsening, start IV insulin bolus+ inf 0.1u/kg
- Weaning off insulin infusion: calculate total dose 24hr insulin, give 50% as long acting (Lantus)
Lines/Tubes/Skin
- Review line locations and date of insertion
- Lines that appear red or inflamed should be moved to another site
- De-escalation of central lines should occur once patient is off pressors and sufficient peripheral access is available. This should be discussed daily.
- If not requiring frequent ABGs, removal of A-lines should occur once pressor requirements are minimal and blood pressure cuff is correlating well.
- Review whether Foley is indicated
- Can keep for patients who are immobile, sedated, or paralyzed. Keep if you need hourly urine output monitoring. Keep for obstruction.
- Remove foley if patient off of heavy sedation and does not need for any of the above reasons.
- Trial of void is essential. Consider Tamsulosin if history of BPH.
Family and Code Status
- Daily updates for family over the phone
- If change in clinical status re-address code status with family
PDF Daily rounding sheet
 |
Steven Johnson, DO Dr. Johnson is a PGY3 and Chief Resident in Emergency Medicine at NS/LIJ. |
 |
Daniel Jafari, MD Dr. Jafari is an Assistant Professor and Attending in EM and surgical critical care attending at NSUH. |
 |
Daniel M. Rolston, MD, MSHPM Dr. Rolston is the Director of the Division of Critical Care Department of Emergency Medicine at Zucker SOM/Northwell. |