[et_pb_section admin_label=”section”][et_pb_row admin_label=”row”][et_pb_column type=”3_4″][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Case
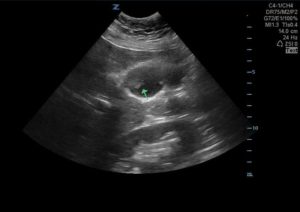
A 46 year old female with a past medical history of hypertension and fibroids presented with cough, fever, emesis, and epigastric pain. She was found to have epigastric and right upper quadrant tenderness to palpation. On bedside gallbladder ultrasound, there were no signs of acute cholecystitis, but a 1.3 by 0.6 cm enhancing lesion was noted within the gallbladder lumen without posterior shadowing.

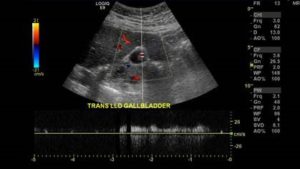
Follow up radiology ultrasound demonstrated the mass with associated vascularity suggestive of neoplasm:
Our patient was admitted for further evaluation with CT and MRI that showed multiple enhancing polypoid lesions in the gallbladder with no associated abnormality involving gallbladder wall or adjacent liver as well as a cystic lesion in the pancreatic head with enhancing internal septations. The patient was discharged with oncology follow up.
Discussion
Gallbladder masses are difficult to diagnose by imaging alone. The reported incidence of these polyps has increased recently due to the ubiquity of ultrasound exams.
The differential includes benign and malignant conditions including:
- Benign:
- Cholesterol polyp
- Adenomyoma
- Inflammatory polyps
- Adenoma
- Malignant polyps:
- Adenocarcinoma (more common than benign adenomas)
- Mucinous cystadenoma
- Squamous cell carcinoma.
- Adenomyomatosis (benign lesion with malignant potential)
Cholesterol polyps originate from cholesterolosis, the accumulation of lipids in the gallbladder wall. Cholesterol deposition leads to a yellow and red discoloration often referred to as “strawberry gallbladder.” The polyps are attached to the gallbladder mucosa by a fragile epithelial layer and can detach and cause pathology similar to gallstones. Additionally, all polyps have the potential to cause biliary colic pain due to prolapse into Hartmann’s pouch (infundibulum of the GB) during gallbladder ejection. It has been postulated that polyps, cholesterolosis and adenomyomatosis restrict gallbladder emptying and can lead to dyspeptic symptoms.
The size of the polyp correlates with risk of malignancy. Polyps greater than two centimeters are assumed to be malignant, and often advanced. Coexistence of primary sclerosing cholangitis, concomitant gallstones and age greater than 50 years are also associated with higher risk for malignancy.
Polyps can be well described on ultrasound. They are single or multiple echogenic foci that do not create shadowing, are not fixed and therefore are not gravity dependent. In adenomyomatosis, there is also focal thickening of the gallbladder wall greater than 4 mm. Spectral doppler ultrasound can increase the accuracy of an imaging guided diagnosis by demonstrating a doppler signal with a specific arterial flow velocity. CT imaging can help with staging gallbladder cancer invasion and metastases. Endoscopic ultrasound (EUS) and CT colonography also have demonstrated promising initial results in diagnosing polyps, but more research is needed. Although there is no current research regarding gallbladder polyps detected by point-of-care ultrasound in the Emergency Department, one large study by Corwin et al recommends follow-up for incidentally found polyps larger than 6mm.
Symptomatic polyps are managed by cholecystectomy. Those with concerning signs for malignancy such as concomitant gallstones, large polyps or Primary Sclerosing Cholangitis are also managed surgically. Recommendations vary according to source, although it is generally recognized that polyps greater than 10 mm require cholecystectomy as gallbladder cancer is highly fatal (10% 5-year survival). Smaller lesions may be observed with serial ultrasounds.
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Conclusions
- Gallbladder polyps are common incidental findings
- Polyps have the potential to cause multiple pathologies including dyspepsia, biliary colic, acute cholecystitis, cholangitis and pancreatitis even without the presence of gallstones.
- As there is a risk for aggressive malignancy associated with polyps, emergency physicians should be aware of malignancy risk factors, and can be integral to the referral and treatment process. Although there is no ED specific evidence yet, one large study by Corwin et al recommends follow-up for incidentally found polyps larger than 6mm.
[/et_pb_text][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Citations
- Andrén-Sandberg Å. Diagnosis and Management of Gallbladder Polyps. North American Journal of Medical Sciences. 2012;4(5):203-211. doi:10.4103/1947-2714.95897.
- Corwin, Michael T. Siewert, Bettina. Sheiman, Robert and Kane, Robert. Incidentally Detected Gallbladder Polyps: Is Follow-up Necessary? —Long-term Clinical and US Analysis of 346 Patients. Radiology 2011 258:1, 277-282
- Kane CF, Brown C, Hoerr S. Papilloma of the gallbladder; report of eight cases. Am J Surg 1952; 83:161.
- McGregor, J. C. and Cordiner, J. W. (1974), Papilloma of the gallbladder. Br J Surg, 61: 356–358. doi:10.1002/bjs.1800610506
- Terzi C, Sökmen S, Seçkin S, et al. Polypoid lesions of the gallbladder: report of 100 cases with special reference to operative indications. Surgery 2000; 127:622.
[/et_pb_text][/et_pb_column][et_pb_column type=”1_4″][et_pb_team_member admin_label=”Person” name=”Miles Gordon, MD” position=”Author” image_url=”http://theempulse.org/wp-content/uploads/2016/04/milesgordan.png” animation=”off” background_layout=”light” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Dr. Gordon is an Emergency Medicine Resident Physician at Northwell Health.
[/et_pb_team_member][et_pb_team_member admin_label=”Person” name=”Dr. Josh Guttman, MD, FRCPC” position=”Reviewer and Ultrasound Editor – theEMPulse.org ” image_url=”http://theempulse.org/wp-content/uploads/2015/10/Guttman-e1453253661766.jpg” animation=”off” background_layout=”light” twitter_url=”https://twitter.com/josh_guttman” use_border_color=”off” border_color=”#ffffff” border_style=”solid” saved_tabs=”all”]
Dr. Guttman graduated from the at Mt. Sinai Medical Center Emergency Ultrasound Fellowship and is now an Attending Physician at the LIJ Division of Emergency Ultrasound.
[/et_pb_team_member][/et_pb_column][/et_pb_row][/et_pb_section]