[et_pb_section][et_pb_row][et_pb_column type=”3_4″][et_pb_text admin_label=”Text” background_layout=”light” text_orientation=”left” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Have you done this? I’m sorry, but it was probably wrong.
A 46 year old woman, M. Iokay, with a history of hypertension presents to your Emergency Department complaining of a Right sided headache, facial asymmetry, speech change, and malaise.
Her vital signs at triage are HR 94 BP 175/104 RR 16 T 97.2 FS 108. A Stroke Code evaluation is called and the ED attending and Neurology stroke team respond. The patient states that she woke up well, but after breakfast began to feel “strange” and “faint.” She reported a gradually worsening Right sided headache and then a family member pointed out that her face looked different. Over the next hour, she felt her speech had changed, and she had measured her BP at 185/100 so she decided to come in. She walked in to the ED from her sister’s car.
The Neuro team notes that Ms. Iokay can wrinkle her forehead bilaterally. Additionally, she has a significant Right lower facial droop (garnering 3 points on the NIH-Stroke Scale) and, possibly, mild dysarthria as the pt’s words are clearly understood but she feels that she doesn’t sound like herself and her mouth feels “numb.” A CT head is read as “possible early grey-white matter border” changes to L hemisphere, correlate clinically. The earliest time of onset is placed at ~2 hrs. PTA, and the team recommends t-PA for her new onset sx, with NIHSS of 3-4.
I do not mean this post to raise arguments over evidence for and against t-PA. I do not mean to raise eyebrows over giving the drug to lower and lower stroke scores. I DO mean to leave you with 2 things:
- Please try not to give t-PA to headaches. Strokes don’t cause pain. That is, pure ischemic strokes will present with neurologic findings without headaches. Have you seen a CVA present with severe headache? Of course you have. You remember it because of the oh-so-impressive CT head. That’s because blood, edema, and midline shift DO cause headache. But if you’re about to t-PA your patient, we can all agree that there’s nothing of concern on that scan.
- I know the CT finding is worrisome, but clinical context is everything. If you thought that stroke was clinically likely, the CT read means a lot. But – since the patient’s chief complaint is HA – in this case you should recall that testing lower and lower pretest probability will inevitably increase false positives.
So what does our patient have? She has a subtle Bell’s palsy, a condition which IS associated with pain on the ipsilateral side of the condition, commonly near or behind the ear. A pt. such as this can have very mild upper facial palsy which can be missed on your rapid cranial nerve exam (and was missed by our experienced Neurology colleagues). Pro-tip? Have the patient squeeze their eyes tightly, and you will see that on the full strength L side, the eyelashes are retracted whereas on the weak orbicularis oculi on the R, there is near full length lash protruding:
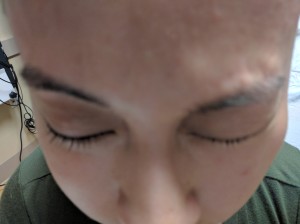
Reproduced with consent of patient
If your patient with a significant headache complaint has an unexplained bonafide neurologic finding after their negative head CT? The next step should be a CT-angiogram of the neck, looking for carotid dissection, a disease that typically will present with neck pain or headache. The next step should NOT be t-PA. If your pt. with HTN and an elevated BP during their stroke eval has HA… well, please don’t just blame the headache on the BP. Please?
For more on headaches and CVA, I would direct you to:
http://www.ncbi.nlm.nih.gov/pubmed/27105768: which describes HaNDL, an alternative dx that looks like stroke but gets better without t-PA.
http://www.neurology.org/content/84/14_Supplement/P1.304: which reports that pts. presenting with headache receive t-PA less frequently than those who do not (thank goodness!).
[/et_pb_text][/et_pb_column][et_pb_column type=”1_4″][et_pb_team_member admin_label=”Person” saved_tabs=”all” name=”Pinaki Mukherji, MD” position=”Program Director, Emergency Medicine, LIJ Medical Center” image_url=”http://theempulse.org/wp-content/uploads/2015/09/dr-pinaki-mukherji-md-11313705.jpg” animation=”off” background_layout=”light” twitter_url=”https://twitter.com/ercowboy” use_border_color=”off” border_color=”#ffffff” border_style=”solid”]
Dr. Mukherji is the Residency Director at LIJ Medical Center in New Hyde Park, NY. He spends most of his time confusing residents and trying to convince doctors that they overestimate the benefits of treatment and underestimate the harms. He has a passion for education and trying not to do things wrong.
[/et_pb_team_member][/et_pb_column][/et_pb_row][/et_pb_section]