Case
63 year old male presented to the ED with left elbow swelling for a few days. The patient was afebrile but the erythema was concerning for cellulitis and a collection around the medial aspect of the elbow. The ultrasound showed a small pocket containing hyperechoic tophi, suggestive of gout, although no drainable collection was noted so the joint was not aspirated. The patient did not have a history of gout and in the presence of significant leukocytosis, the patient was treated with antibiotics. The patient was admitted for cellulitis, found to have bacteremia during his hospital stay, and treated for 28 days.
Example image was attained from http://www.jultrasoundmed.org/
Discussion
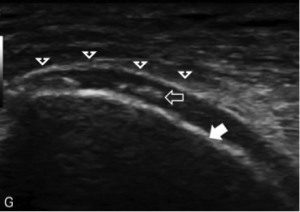
While the diagnosis of gout via joint aspiration was not made in this particular case, it brings an important opportunity to discuss findings on ultrasound suggestive of gout and the supporting literature. Thiele and Schlesinger (2) studied the utility of ultrasound in the diagnosis of gout. They performed a retrospective study, reviewing the images of patients with proven gout compared with matched controls. The features that they searched for included hyperechoic irregular bands found in the joint spaces as well as the “double contour sign” (see image) which depicts the urate deposition as an irregular echogenic line over the most superficial hyaline cartilage. They found that these were found in 92% of patients with gout and in none of the controls with a p value of <0.001. Furthermore, they found that erosions can also be seen by ultrasound. The overall conclusion of the study was that ultrasound may be a reliable noninvasive method of diagnosing gout. Major criticisms of the study include its small size, as well as selection bias in that these were rheumatology patients. Therefore, it is difficult to determine what the generalizability of this study may be to the emergency department.
In 2013, Girish et. al (3) wrote a review article looking at different imaging modalities in gout. The double contour sign described above has been shown to be 25% to 95% sensitive across multiple studies. The authors pointed out that most studies to this point have been small and failed to provide reliable sensitivity and specificity measures to the sonographic findings associated with gout.
A recent study from Pascal et. al. (4) looked at the utility to ultrasound in diagnosis of gout and Calcium pyrophosphate (CPP) arthritis (pseudogout). They prospectively looked at 109 patient presenting with acute arthritis. The results showed that looking at multiple joints increases sensitivity from 60 to 84% in gout and 60 to 81% for CPP with sensitivity dropping significantly from 92 to 78% in gout and 80 to 62% for CPP. Overall, the study concluded that while ultrasound does provide some diagnostic utility when examining multiple joints, arthrocentesis is still the gold standard in the diagnosis of gout and CPP. Looking at multiple joints also may not be practical in an ED setting with limited time available for performance of the ultrasound
Conclusion
Some evidence does exist that gout has sonographic findings that may suggest its presence in the appropriate clinical context, however literature lacks robust evidence that this indeed could be used reliably as a diagnostic tool. Additionally, septic arthritis is more common in joints with gout and therefore finding gout on ultrasound does not rule out septic arthritis, as the two may co-exist. Therefore, in our case described above the patient was likely treated appropriately given other clinical findings that suggested cellulitis, and may simply warrant an outpatient rheumatological workup, especially if further flare ups occur.
References:
- Journal of Ultrasound in Medicine. <http://www.jultrasoundmed.org/>. August 20 2015.
- Thiele RG, Schlesinger N. Diagnosis of gout by ultrasound. Rheumatology (2007) 46 (7):1116-1121.
- Gandikota Girish, David M. Melville, Gurjit S. Kaeley, et al., “Imaging Appearances in Gout,” Arthritis, vol. 2013, Article ID 673401, 10 pages, 2013.
- Pascal Z, Valcov R, Fabreguet I, Dumusc A, Omoumi P, So A. “A Prospective Evaluation of Ultrasound as a Diagnostic Tool in Acute Microcrystalline Arthritis. Arthritis Res Ther. 2015;17(188).
Reviewed by Dr. Joshua Guttman